ABOUT ENDOSCOPIC SPINE SURGERY:
PETER VAN DAELE TECHNIQUE
INDIA'S NO. 1
ENDOSCOPIC SPINE SURGERY CENTRE
- Walk in one hour
- No bed rest
- Out of hospital same day
- MAGIC...
1500+ ENDOSCOPIC SPINE SURGERIES
No complications in Orthopaedics till now
(In expert hands of Dr. Harprit)
SUPER SPINE MASTER - Dr. HARPRIT SINGH

MANAGING DIRECTOR AND CHIEF ORTHOPAEDIC SURGEON
DR. HARPRIT SINGH
MBBS, MS (Ortho)
4 Gold Medals and 3 Silver Medals
4 Distinctions

Dr. Harprit Singh with the master of Endoscopic Spine Surgery Dr. Peter Van Daele at OLV Hospital, Belgium.
- An average surgeon would quickly adopt to this transforminal technique and put a title ENDOSCOPIC SPINE SURGEON under his name. And he will try to do all cases by this technique while actually 1 in 100 cases requires the approach. That’s the reason of failing of Endoscopic Spine Surgery in their hands. While INTERLAMINAR Approach requires high grade training and expensive equipment.
ENDOSCOPIC SPINE SURGERIES
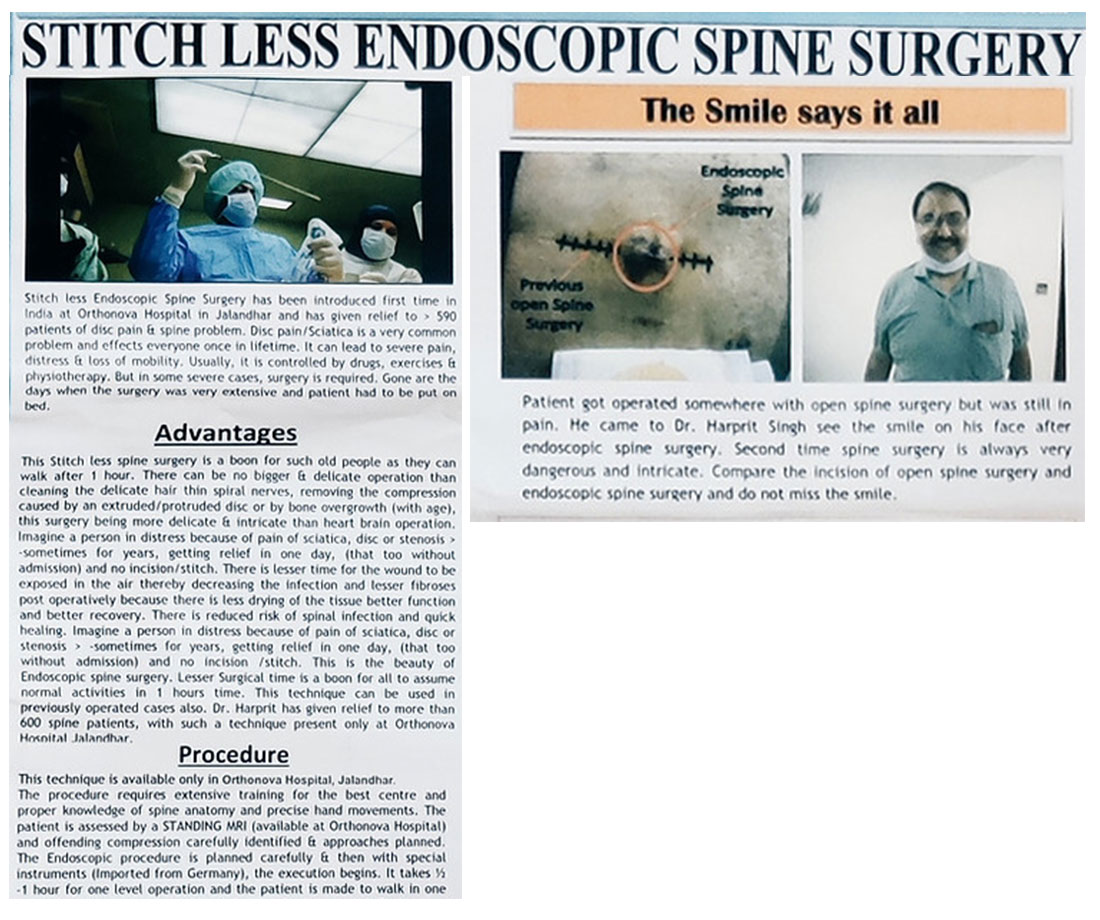
Dr. Harprit performing Stitchless Endoscopic Spine Surgery which is a much higher and precise technique than MIS.
Watch his eyes, that are never off the camera-rest everything is automated.
Fmr Mayor of Chandigarh, sharing her views after getting spine surgery at orthonova. She wants such clean hospitals in Chandigarh
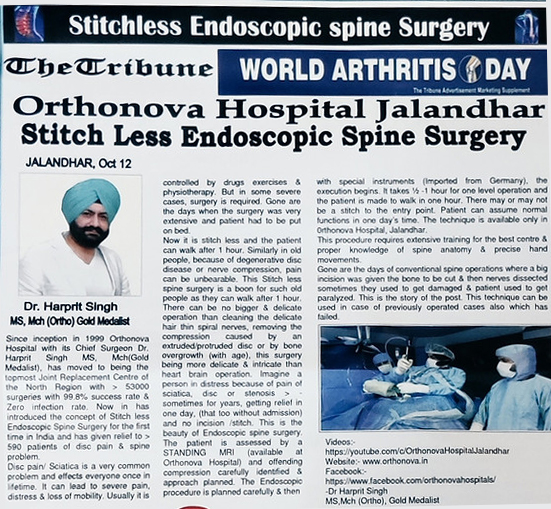
Cervical Spine Endoscopy.
The most delicate surgery.
Only 2 centres in India offering this.
Van Daele tech.
Walking after 1hr.
THE FULL - ENDOSCOPIC TRANSFORMINAL TECHNIQUE :


One is the easy type & more common, but not precise, it is called the Transforminal (Inside out) Technique. It is an easy procedure therefore, it is practiced by most of the surgeons because its indications are very limited. You cannot do it in all the cases (may be 1 out of 100 cases).
So, most of the surgeons start the Endoscopic Spine Surgery by Transforminal approach but they give up too soon.
ADVANTAGES:
- Can be done in relatively cheap setup.
- No anesthesia is required.
- No special instrumentation is required.
So, most of the surgeons find it easy to do it. This matches:-
- Complete disc removal is not possible with this approach.
- Decompression of the spine cannot be done. Laminectomy cannot be done.
- If the disc protrusion is in mid line, the disc cannot be removed.
So, Transforminal Endoscopy is effective in only one indication :-
When the disc is extruded formally (i.e.) Femoral disc extrusion and which is pressing on the nerve then only this can be taken.
But the surgeon who knows this approach will try to put all the cases in this approach.
That’s why the Transforminal Endoscopy fails because the indication is only extruded femoral disc.
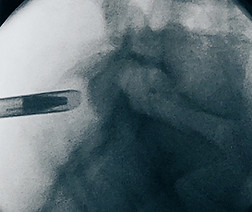
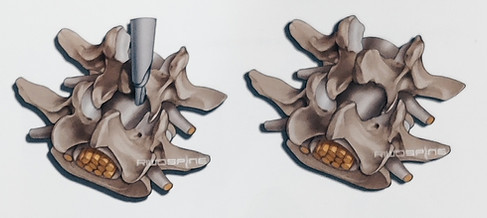
OPERATING PROCEDURE :

The endoscope is inserted through the working sleeves.
The lateral access enables partial endoscopic inspection of spinal cord.

THE FULL - ENDOSCOPIC INTERLAMINAR TECHNIQUE
The real ENDOSCOPIC PROCEDURE



The second approach also the real Endoscopy is a different procedure. You need special training for this procedure. It cannot be done in regular setup. It needs a dedicated setup for this. It is a mid line approach.
Transforminal approach is side approach. In Transforminal approach you have to go from side Lumbar area and in Interlaminar, you have to go right at the center.
ADVANTAGES:
-
We can do the following procedures:-
- Laminectomy.
- Decompression.
- Removal of foraminal disc.
- Removal of mid line disc.
- Removal of disc which has migrated upwards.
- Removal of disc migrated downwards.
- Removal of cyst.
- Removal of extramedullary tumors.
- Clearing of tubercular pus.
DISADVANTAGES:
- Special instrumentation is required.
- Anesthesia is highly specialized.
- Special training is required for this procedure.
- Done in very few centres over the world.
- Direct access to the epidural space with continous visualization is hence necessary for adequate operataions within the spinal canal. A lateral access is necessary for this when using the full-endoscopic transforaminal technique. The bony and neural borders of the neuroforamen define limits for mobility and hence also in relation to the indication criteria. Furthermore, the necessary lateral access in the lower levels may be prevented by the pelvis. On the basis of our experience, these restrictions encompass a spectrum of pathologies which are not operable using the full-endoscopic transforminal approach due to technical limitations.
- The light and imaging system with 25 direction of view is located directly in the relevant working area so that traumatization can be minimized in the access passage and also in connection with the structure of the spinal canal. Working in a continous flow of liquid provides excellent visibility conditions.
- Mobility for the new endoscope is achieved by handling with joystick technology. Protection of the neural structures is provided by manipulating the bevelled operating sleeve like a nerve hook. In combination with the newly developed instrument sets, this represents a genuine minimally invasive procedure.
- Indications primarily relate to pathologies within the spinal canal. It is important to note that the size of the interlaminar window can prevent free passage of the endoscopic. In this case, the bone can be cut until the target point is reached without opening the ligamentum flavum or damaging the zygoapophyseal joint.
- In most cases, bony resection should be avoided, although the pathology precludes this in the case of spinal canal stenoses. The incision in the ligamentum flavum can be reduced to a few millimeters because the elasticity of the ligament facilities enrty into spinal canal. On the other hand, mobility to the other side is equivalent to conventional operations.
- In a craniocaudal direction, access along adjacent levels can be considered in order to minimize the recection of structures of the spinal canal. The full-endoscopic interlaminar technique permits selective operation of pathologies within the spinla canal with minimized acccess-related traumatization. The transforaminal access is generally the most appropriate for intradiskal, intraforaminal or extraforaminal working.
- The transforminal procedure has more restrictions compared with the interlaminar approach, although it provides the best tissue conservation. The anatomical and pathological conditions mean that the percentage of transforminal to intralaminar procedures is approx 40 to 99 in practice.
Full-endoscopic Interlaminar Access

Handling the telescope using the joystick principle permits mobility.
The interlaminar access gurantees outstanding visibilty for the structures of the spinal canal.
POSITIONING:
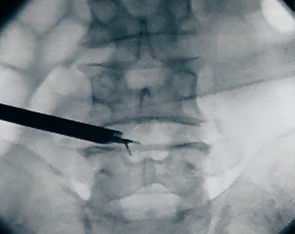
The patient is in the prone position lying on a pelvic and thorax roll on an X-ray permeable table.
Application of a C- arm is required during the operation.

Marking the entry point on the skin.
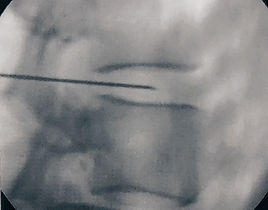
Entry point should be in a maximally median position.
Determination of the access:
The access is determined under X-ray control on the basis of the anatomical landmarks in the AP view and taking account of the pathology. It must be positioned maximally medially in the interlaminar window in order to permit entry under the obliquely positioned zygaopophyseal joint literally.
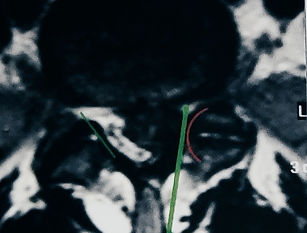
Entry under the zygoapophyseal joints should be faciliated.
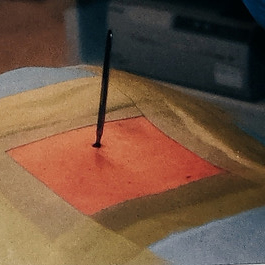
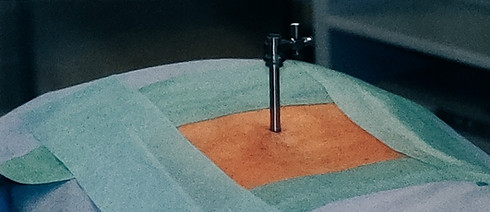
Stab Incision
Implementation of the process:


After determining the entry point in the skin and carrying out the stab incision the dilator is inserted under AP X-ray control unit the ligamentum flavum. The subsequent procedure is then performed in the lateral X-ray view. The working sleeve with oblique opening is pushed through the dilator toward the ligament and the dilator is removed.
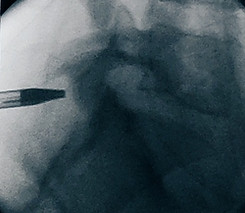
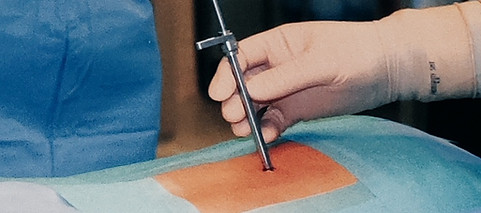
Insertion of the dilator and then the sleeve under image intensifier control to the ligamentum flavum.
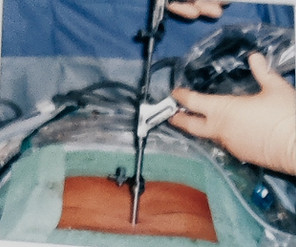
Operating Procedure:

The endoscope is inserted through the working sleeve. The operation is carried out under endoscopic vision using different instrument sets positioned through the intraendoscopic working channel and with a continous flow of liquid.
After opening the ligamentum flavum, it is possible to enter the spinal canal. Mobility with the endoscope is achieved via handling in the joystick principle. Protection of the neural structures is provided by the beveled working sleeve as a second instrument and through rotation.


The beveled working sleeve can be used as a second instrument by rotating.


The locking caps for the telescope and working sleeve should only be used briefly if bleeding obscures visibility since when operations last a long time and the drainage of fluid is prevented without being noticed, the consequences of volume overload and elevated pressure within the spinal canal and the associated and neighboring structures cannot theoretically be completely excluded.
An extended and uniterrupted excessive retraction of the neural structures with the working sleeve in a medial direction must be avoided particularly in cranial areas, or only carried out intermittently, in order to avoid the risk of neurological damage. Experience indicates that generally speaking there is an increased risk of complications occuring when all new procedures are carried out, in particularly during the learning curve.

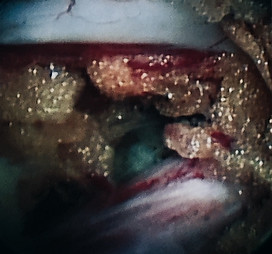
Opening of the ligamentum flavum

View of the axilla at L5/S1

A necessary bone resection is possible with the instrument and burrs available.

The interlaminar access permits working in the spinal canal in vision.
Bone resection may be necessary in order to expand mobility within the spinal canal or if there are problems during access. That may be the case e.g. in sequestered spinal disk herniations, small interlaminar windows or during an operation on recess stenosis.
After the access has been implemented, the bony structures are dissected. It may be helpful to start decompression at the caudal end of the descending factes. Medial structures of the descending facets or the caudal and cranial laminas may be resected depending on the pathology.

It may be helpful to start decompression at the caudal end of the descending facets.
The extent of bony resection depends on the pathology.
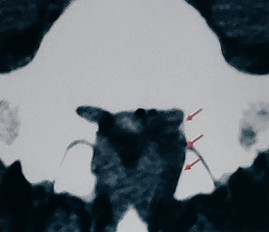
A range of burrs and bone punches are available for bone resection which can be inserted through the intraendoscopic working channel.

Lateral bone resection is carried out on the floor of the spinal canal directly in the working area.

